
Alaska Internal Medicine Rural Residency
University of Washington School of Medicine (Soldotna) ProgramAlaska Internal Medicine Rural Residency
Overview
The University of Washington Alaska Internal Medicine Rural Residency Program is the nation’s first ACGME-accredited program of its kind. It offers the best of both worlds by combining the educational expertise of a well-established urban academic program with a novel primary care training experience in rural Alaska.
1-2 Model
The program will follow the 1-2 model common among rural training programs in family medicine. The first year will be spent integrated with the University of Washington Internal Medicine Residency Program in Seattle, WA. Our residents (2-2-2) will be embedded in the primary care cohort for their intern year, getting excellent training in the core clinical skills for primary care, inpatient medicine, intensive care, neurology, and geriatrics.
Our residents will then move to the rural community of Soldotna, Alaska for their second and third years. In Soldotna, residents will have an intensive longitudinal outpatient experience, including four half-days per week of continuity clinic providing primary care and internal medicine consultation to a panel of medically complex patients. They will spend additional months in Alaska doing core and elective rotations at other rural and urban sites throughout the state, allowing them to get broad-spectrum general internal medicine training, as well as exposure to diverse clinical opportunities available for future practice.
Rural primary care
In contrast to more traditional IM programs, this program is particularly focused on training residents to be strong rural primary care providers, with a honed skill set that allows them to care for highly comorbid/complex patients in communities with far fewer health care resources than are available in metropolitan areas.
Highlights
- Rural continuity clinic site offers full spectrum outpatient general internal medicine:
- Primary care
- Management of subspecialty problems
- Internal medicine consultation for local family practitioners and surgeons
- Interpretation of cardiac stress tests and PFTs
- Outpatient procedures, including paracentesis, thoracentesis, cardioversion, joint injections, and skin biopsies
- Robust training in non-IM specialty skills that are essential to providing comprehensive primary care in a rural area
- Longitudinal curriculum in Alaska to maximize continuity of care and skill-building
- Small complement to allow for individualized teaching and a highly supportive training environment
- Mentorship from a close-knit team of board-certified internists with well over fifty years combined experience in clinical medicine and education
- Opportunity to teach UW third-year medical students on their IM core clerkship
- High volume of endoscopy for invested learners
- Elective experiences with remote Alaskan communities and tribal health organizations
- Several options for full spectrum jobs on the Kenai Peninsula and throughout Alaska post-residency
Mission
The University of Washington - Alaska Internal Medicine Rural Residency Program (UW AK IM RRP) will provide outstanding general internal medicine training, including an intensive Alaska-based rural primary care experience, with the goal of recruiting exceptional internists to practice in high-need Alaskan communities.
Vision
UW AK IM RRP graduates will improve the health of rural and urban Alaskans by providing primary care to patients with complex medical problems; offering internal medicine consultation, as well as coordination of care with medical subspecialists, when subspecialty care is difficult to access; and serving in educational and leadership roles within their medical communities.
Postgraduate Year 1
The first year of training will feature a traditional block schedule model with multiple inpatient rotations, immersion blocks for primary care skill building, and a continuity clinic experience at General Internal Medicine & Women’s Health Care, VA Puget Sound.
VA Continuity Clinic
- The VA continuity clinic offers residents the opportunity to become comfortable caring for patients with multiple diseases and co-morbid conditions.
- Residents will engage in team-based, patient-centered care focusing on a personalized, integrated, comprehensive, and coordinated approach to health care through the VA’s patient-centered medical home model.
Outpatient GIM Immersion Blocks
- Mornings will include didactic sessions on the management of common conditions, physical exam, practice management, and patient interactions. These sessions are followed by interactive sessions including journal club, chart review, and “report.”
- Afternoons will be spent at the continuity clinic site caring for a panel of primary care patients.
Block Diagram for PGY1
Each block is a 4-week rotation. Blocks with two sites or rotations listed are split into 2-week rotations. Residents will have 28 days of vacation. There is one elective opportunity.
| Block | Site | Rotation |
|---|---|---|
| 1 | UWMC | Inpatient Medicine |
| 2 | HMC | Inpatient Medicine |
| 3 | HMC | Cardiology |
| 4 | HMC | Geriatrics |
| 5 | HMC | VA | Neurology |
| 6 | VA | MICU |
| 7 | VA | Inpatient Medicine |
| 8 | VA | Outpatient GIM Immersion |
| 9 | VA | Outpatient GIM Immersion |
| 10 | VA | Renal |
| 11 | VA | Pulmonary |
| 12 | VA | Hematology-Oncology |
| 13 | All Sites | Risk | Elective |
Postgraduate Years 2 & 3
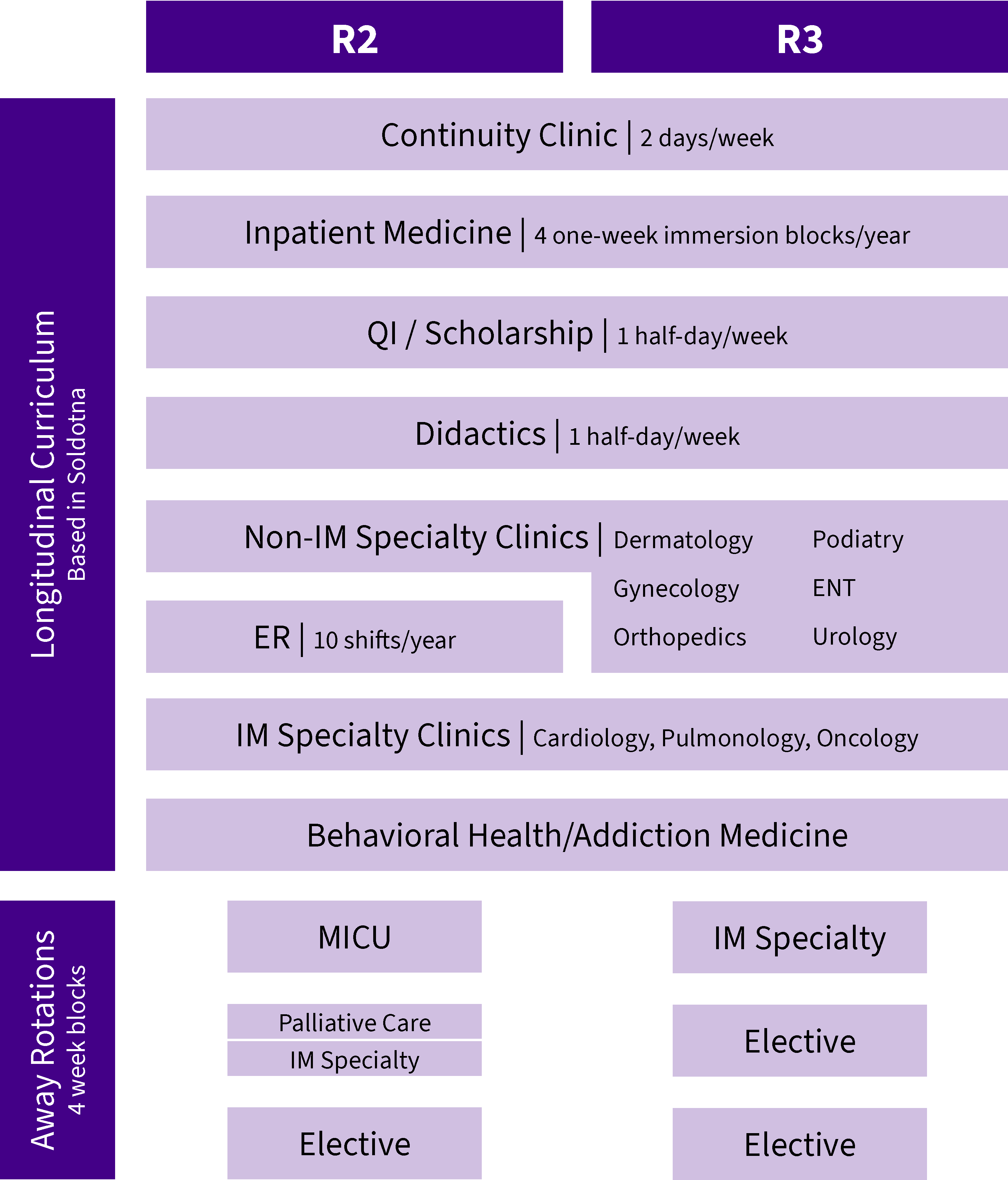
Longitudinal Integrated Curriculum
Residents will have a fully integrated longitudinal curriculum during their second and third years. This innovative curriculum will allow residents to maximize continuity in both their general medicine clinic and other clinical settings, including IM and non-IM specialty clinics, the inpatient service, and behavioral health. It also will allow residents to better experience what life is like as a practicing physician. This curriculum caters to engaged, independent adult learners and will allow for flexibility with electives and special interests/projects.
Continuity Clinic
Residents will provide primary care and specialty consultation for a panel of medically complex patients at Central Peninsula Internal Medicine (CPIM). This longitudinal outpatient experience will involve at least two full clinic days per week over nine of thirteen curricular blocks each year.
CPIM was established in 1991 with a goal of providing high quality medical care to patients on the Kenai Peninsula. The practice has grown with the Central Peninsula community and now includes four board-certified physicians and two certified nurse practitioners. All of our clinicians enjoy strong relationships with colleagues throughout the local medical community, with other Alaskan medical institutions, and with the University of Washington School of Medicine. CPIM has served as a clinical teaching site for UW IM residents and third-year IM core clerkship students since 1994.
Inpatient Experience
Residents will round on their primary care patients in the hospital and rehab facility and will have four 1-week inpatient immersion experiences at Central Peninsula Hospital (CPH) each year. There will be a one-month MICU rotation in Anchorage during the second year as well. Residents will not lead a traditional inpatient teaching team but instead partner with interdisciplinary care team members while learning how to be an independent clinical decision-maker in the inpatient setting, which is the practice model throughout rural Alaska.
Specialty and Subspecialty Care
Residents will have the option to rotate regularly at local cardiology, pulmonology, and/or oncology clinics and will receive longitudinal integrated medical subspecialty precepting for their own patients.
Residents also will rotate through non-internal medicine specialty clinics, including gynecology, orthopedics, dermatology, podiatry, urology, and otolaryngology, so that they can learn the additional skills that are essential to providing comprehensive primary care in a rural area.
Behavioral Health
Residents will participate in longitudinal training that includes psychiatry clinic, rounds at the local transitional care facility, addiction medicine clinic, and training in buprenorphine management.
Electives
Residents will have 4-8 weeks of rural-based electives per year. Elective time can be spent at rural sites throughout Alaska, including the home base of the Kenai Peninsula. These electives, at sites such as Bethel, Nome, Juneau, and Sitka, will give residents the chance to explore the diverse practice opportunities available throughout the state.
Didactics
Residents will participate in small and large group didactic sessions, some in partnership with the UW IM categorical and primary care programs, on a weekly basis.
Scholarship
Residents will complete a quality improvement or other scholarly project and will develop panel management skills over the course of their two years in Alaska.
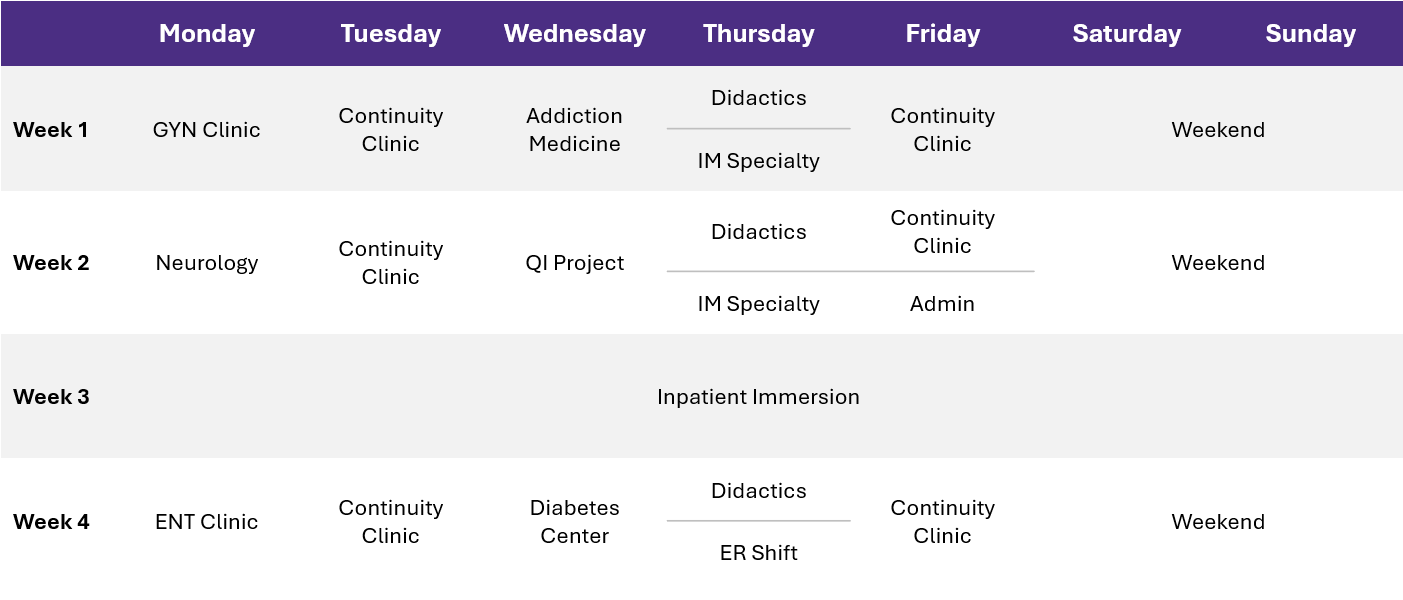
Block Diagram for PGY2 & PGY3
Sample 4-Week Schedule for PGY2 & PGY3
We are dedicated to enhancing the diversity of our housestaff and faculty to reflect the diversity we aim to cultivate within the residency, as well as the diversity inherent in a program that includes both rural and urban core training sites. We are committed to educating our residents about the inequities diverse patients continue to face.
As residents move through our program, didactics will include annual training in diversity awareness and cultural competency, and professional development activities will take full advantage of the diverse clinical, scholarly, and educational opportunities available within Alaska and the broader UW system. Additionally, the program will offer elective clinical rotations at sites that reflect Alaska’s diverse communities, including sites run by Alaska Native tribal governments.